Project completed as part of the Northampton General Hospital NHS Trust Green Team Competition 2024-25.
Team members:
- Jasmine Lowdon (Band 6 IPC nurse, Project Co-ordinator/Project lead)
- Holly Slyne (Associate Director of Infection Prevention & Control, Senior project advisor/mentor)
- Mary Reynolds (Project Admin Support)
- Athira Sreelatha (HCA, project assistant)
Setting / patent group:
Inpatient wards at University Hospitals of Northampton NHS Trust
Issue:
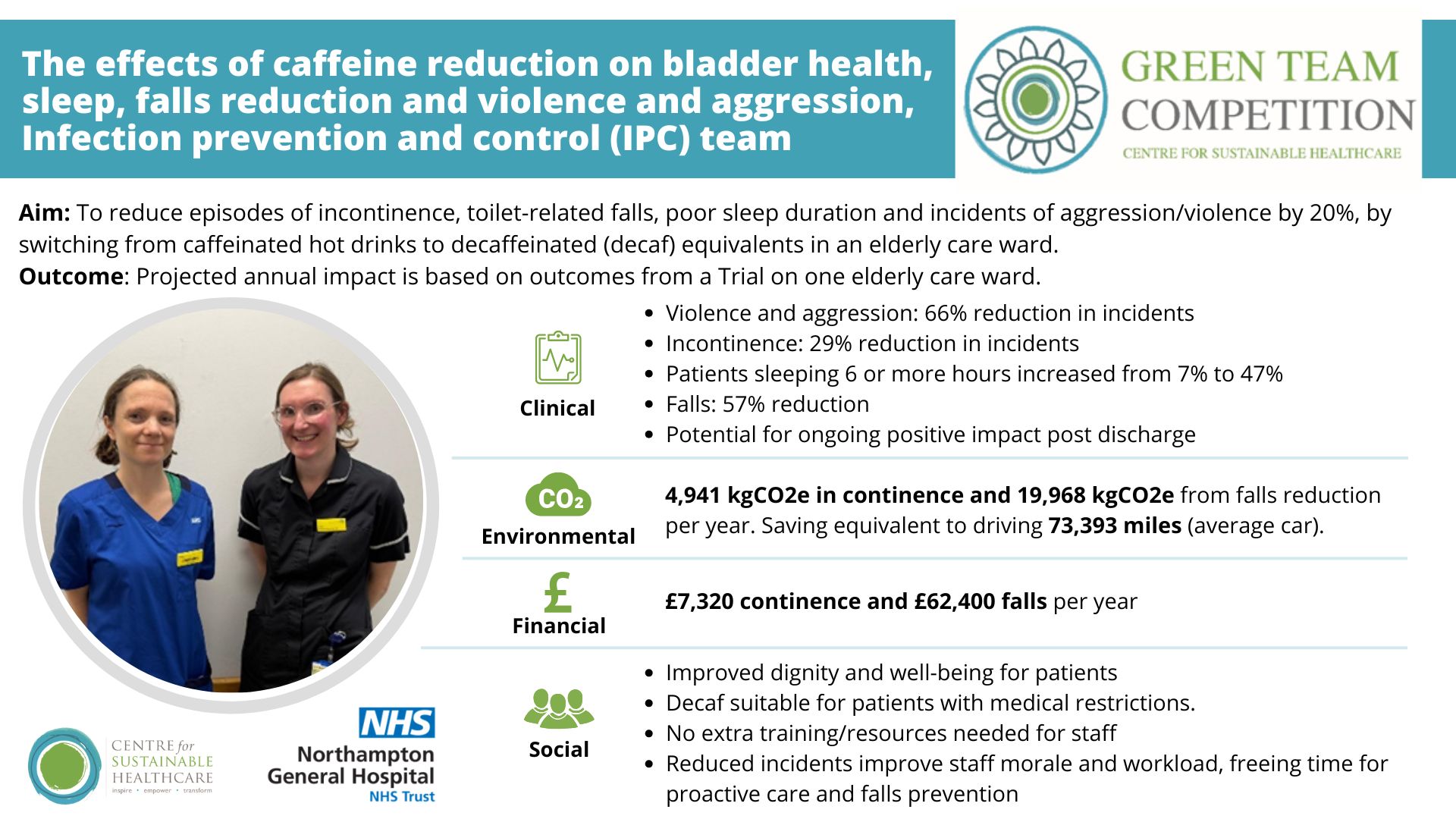
Caffeinated hot beverages, such as tea and coffee, were routinely offered as the default option to inpatients. However, caffeine is a known stimulant with adverse effects on bladder function, particularly in older adults. Its consumption can exacerbate urinary incontinence, increase frequency of toileting, and has been associated with a heightened incidence of falls, disturbed sleep, and behavioural issues such as aggression and agitation. Urinary incontinence contributes significantly to healthcare costs and patient morbidity. At Northampton General Hospital (NGH), expenditure on incontinence aids alone is estimated at approximately £1 million annually. Additionally, incontinence increases the risk of urinary tract infections, dehydration, and skin breakdown, while also placing considerable demand on staff time and resources.
Intervention:
On Brampton and Knightly wards, the default hot beverage was switched from caffeinated to decaffeinated tea and coffee, with patients informed of the associated health benefits. Decaffeinated drinks were supplied in bulk, and discharge plans include educational materials to promote continued consumption post-discharge.
Outcomes:
Environmental
4,941 kgCO2e in continence and 19,968 kgCO2e from falls reduction per year. Saving equivalent to driving 73,393 miles (average car).
Social
The initiative may contribute to improved staff morale through reductions in patient aggression, workload associated with toileting support, bed changes, and managing distress. Enhanced efficiency in staff time allocation allows for greater attention to holistic patient care. Importantly, the intervention requires no additional training or resources for implementation, as decaffeinated beverages are prepared using existing processes. From a patient perspective, the reduction in incontinence and falls supports dignity, mental well-being, and inclusivity, as decaffeinated options are appropriate for all patients, including those with contraindications to caffeine. Offering personalised beverage choices fosters patient trust and enhances the overall care experience.
Clinical
The intervention was associated with notable improvements in patient outcomes. Incontinence rates improved by 29%, and there was a 66% reduction in reported incidents of violence and aggression. Sleep quality also improved significantly, with the proportion of patients sleeping six or more hours per night increasing from 7% to 47% (p = 0.002). Additionally, Brampton Ward experienced a 57% reduction in total patient falls during the study period compared to the previous year, although this may have been influenced by concurrent fall prevention strategies. Improvements in continence may also contribute to a reduced risk of urinary tract infections, dehydration, and skin irritation.
Financial
£7,320 continence and £62,400 falls per year for trial ward.
The initial £30,000 investment for a hospital-wide switch to decaffeinated beverages would therefore be offset by savings in just one ward.
Key learning point:
Switching the default hot drink to decaffeinated options in elderly inpatient settings has been linked to improved clinical outcomes, cost and environmental savings, and enhanced patient dignity and staff morale. The intervention maintains patient choice while promoting inclusivity and sustainability. Continued education and further research are needed to assess long-term impact and broader applicability.
Please log in or sign up to comment.