Project completed as part of the National 2025 Green Nursing Challenge by the Oxford Health NHS Foundation Trust.
Team members:
- Gabbie Parham, Senior Matron, Community Nursing
- Helen Squires, Operations Manager
- Daniel Edwards, Diabetes Clinical Lead
- Charis Smith, District Nursing Locality Lead
- Valentina Georgescu, Advanced District Nurse Specialist
- Julie Humphries, District Nursing Locality Lead
- Alice Jeffries, District Nursing Team Leader
Issue
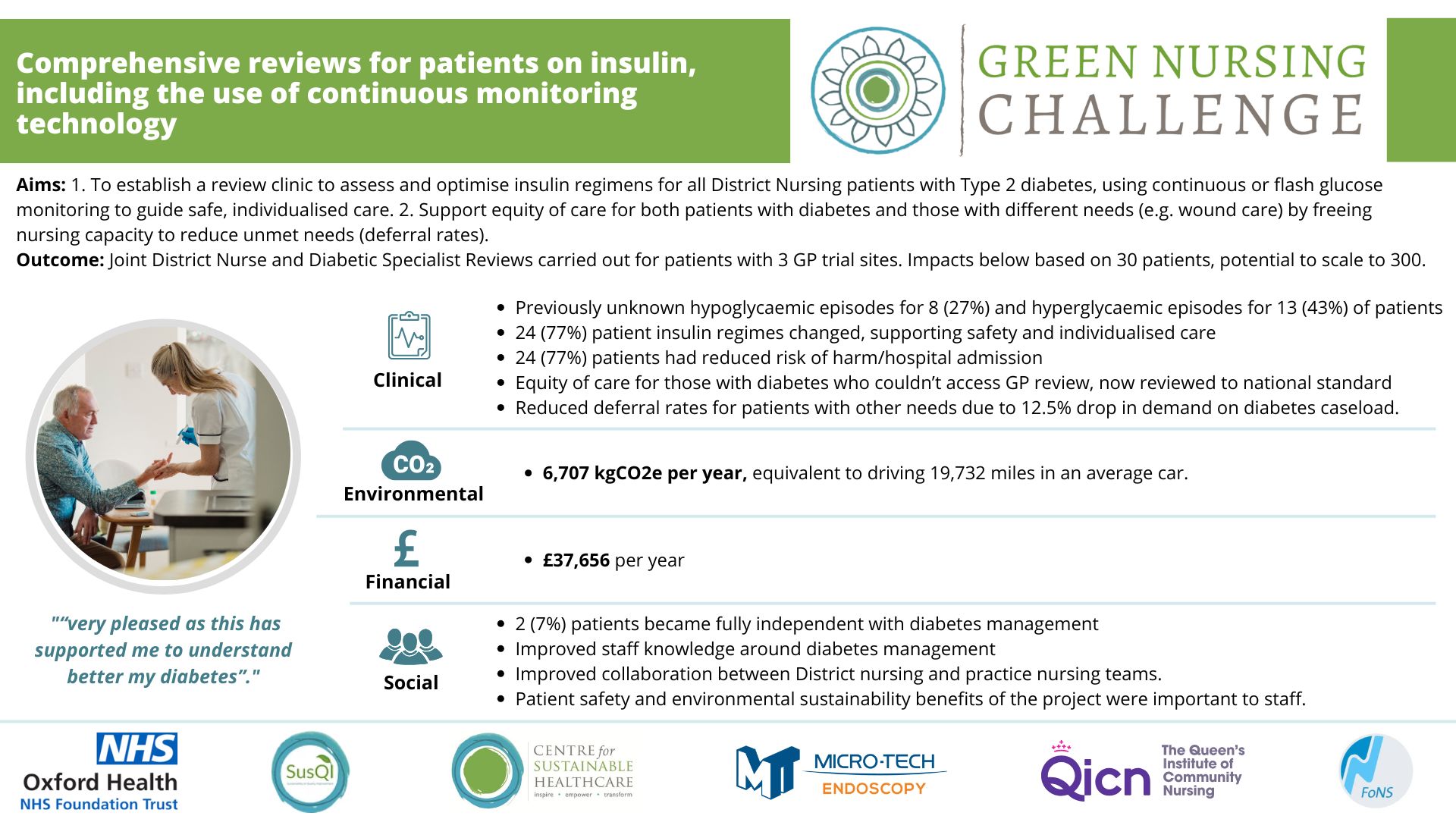
Patients with Type 2 diabetes, who become acutely unwell and need hospitalisation, may have insulin prescribed in hospital, which can continue after their discharge. Oxford Health District Nursing Service has a caseload of around 300 patients across the county of Oxfordshire with diabetes (majority Type 2 diabetes) who are unable to manage their own injections and require daily or sometimes twice daily insulin administration by the District Nursing service. Some of these patients, once they have recovered from their initial illness, do not require insulin to manage their diabetes, or can learn to be self-caring with their insulin regimes. Despite these changes in clinical needs, insulin regimes for these patients may not be reviewed for some time meaning patients continue to have insulin for the rest of their lives. Patients not having a review of their care can lead to life threatening complications such as hypoglycaemia (low blood glucose) and hyperglycaemic (high blood glucose) diabetic ketoacidosis events that require hospital admission.
Intervention
The team established a review process to assess and optimise insulin regimens for all District Nursing patients with Type 2 diabetes, using continuous or flash glucose monitoring to guide safe, individualised care. Their aim was to ensure safe, effective and individualised diabetes management, and avoid the consequences of unstable blood glucose levels. The team hoped their intervention would support equity of care for both patients with diabetes and those with different needs (e.g. wound care) by freeing nursing capacity to reduce deferral rates.
The first change was to commence a joint review project involving both the District Nurse and Practice nursing teams to ensure comprehensive specialist diabetes reviews were undertaken for all patients on the caseload.
The second change saw the implementation of continuous or flash blood glucose monitoring (BGM) technology for all patients being reviewed, to allow fluctuations in blood glucose levels to be monitored over a 24 hour period where hypoglycaemic or hyperglycaemic episodes were picked up by the district nurses then sent on for Practice Nurse review - with subsequent amendments of insulin regimes.
Results:
Joint District Nurse and Diabetic Specialist Reviews carried out for patients with 3 GP trial sites. Impacts below based on 30 patients, potential to scale to 300.
Clinical
Previously unknown hypoglycaemic episodes for 8 (27%) and hyperglycaemic episodes for 13 (43%) of patients
24 (77%) patient insulin regimes changed, supporting safety and individualised care
24 (77%) patients had reduced risk of harm/hospital admission
Equity of care for those with diabetes who couldn’t access GP review, now reviewed to national standard
Reduced deferral rates for patients with other needs due to 12.5% drop in demand on diabetes caseload.
Environmental
Extrapolating the results, the reduction in home visits will lead to annual GHG emissions savings of 6,707 kgCO2e.
Economical
In total, £37,656 in cost efficiency savings are projected per year from reducing 4 appointments a day on the insulin caseload (assuming the sensors are used for 10 days per patient).
Social
2 (7%) patients became fully independent with diabetes management
Improved staff knowledge around diabetes management
Improved collaboration between District nursing and practice nursing teams.
Patient safety and environmental sustainability benefits of the project were important to staff.
Key learning:
Proactive, collaborative reviews of insulin regimens, especially using continuous glucose monitoring, can significantly improve patient safety, reduce unnecessary interventions, and free up nursing capacity. The project demonstrated that integrating primary and community care teams to review housebound patients not only enhances clinical outcomes and equity of care, but also delivers measurable environmental and financial sustainability benefits.
Please log in or sign up to comment.